Hello world,
I’m 38 years old, I have Type 2 diabetes, and I’m going to try to figure out how it works and better ways of managing it through self-tracking, experimentation, and (hopefully) collaborating with
others doing the same thing.
At the age of 29, I started having the following symptoms:
- Insomnia – I started sleeping <4 hours per night, but wasn’t tired during the day
- Weight loss – went from 210 to ~190 lbs. in 1 month without changing my diet
- Thirst – started drinking a ton of water. By the end, ~1 cup every 0.5 h
- Frequent urination – presumably caused by #3
- Blurred vision – had to sit much closer to the screen at a seminar I attended
I went to the doctor and was quickly diagnosed with Type 2 diabetes. My HbA1c was 8.7%, which means that my blood glucose was averaging >232 mg/dL. People without diabetes will have an H1Ac of <5.7 (average glucose <120 mg/dL).
I went home and read everything I could find on diabetes symptoms, progression, and treatment. I found out that since most people get diabetes after age 50, there’s almost no data on long term survival
rates or even disease progression for people my age.
Not wanting to die, go blind, lose my feet, or even have to start injecting with insulin, I decided to treat my diabetes aggressively, with a goal of keeping my blood sugar the same as that of a non-diabetic. I
went on Metformin, started obsessively testing my blood glucose, radically cut down on the amount of
carbohydrates I ate (down to <20 g per meal), and cut calories until I hit 165 lbs. (BMI = 23.5).
With all that, I was able to get my blood sugarunder control. Here’s my HbA1c history for the first two years:
- 3/2011 – 8.7%
- 6/2011 – 6.0%
- 3/2012 – 5.3%
- 8/2012 – 5.3%
So, I got my blood sugar into the “normal” range, but at the cost of having to think about/worry about
food constantly. It was worth it, but very unpleasant.
I was able to maintain this approach for 4 years, but in late 2016 I got pneumonia. My blood sugar was high while I was sick (~160 mg/dL), which wasn’t a big deal, but when I recovered it didn’t come
down. With the same diet as before, I routinely had a fasting blood sugar of >120 mg/dL and 2h post-meal level of >160 mg/dL.
After struggling to try to get things back under control with diet and exercise, I went to a series of doctors and eventually ended up going on insulin. This helped, but I was still seeing blood sugar higher than “normal” and since I my blood sugar was “under control” by the standard of care, the doctors I was seeing didn’t want to prescribe any further treatment.
As when I was diagnosed, I did my own search and ended up finding a book by Dr. Richard
Bernstein that advocated a more aggressive treatment approach involving a strict and consistent low-carb diet and careful, but aggressive use of insulin to keep blood sugar in the range normal for a non-diabetic. I became a patient of Dr. Bernstein’s and by following his approach was finally able to get my blood sugar back under control to my standards.
Here’s my HbA1c history during this time:
- 11/2016 – 6.7% (after recovery from pneumonia)
- 12/2016 – 6.3%
- 2/2017 – 6.0%
- 3/2017 – 6.4%
- 9/2017 – Started working with Dr. Bernstein.
- 9/2019 – 5.1% (most recent)
This new approach works, but at the cost of an extremely regimented diet, exercise, and lifestyle. It also frequently falls apart when I have to travel or eat out for work. Lastly, I’m only 38 and I’m worried about how much more difficult this will get if my diabetes progresses any further.
A few months ago, I started reading about the Quantified Self movement, people who track information about themselves to better understand and improve their mental or physical well-being. I was particularly inspired by the people who used self-tracking to understand and control diabetes (link, link, link). Thinking about it, I realized that while I had my blood sugar under control, I didn’t really understand what influenced my glucose level beyond the simplisitic “more carbs or protein –> higher glucose” and “fiber and sugar alcohols >> sugar and starches”. There’s a lot of “common wisdom,” as well as peer reviewed research on the topic, but much of it is contradictory, doesn’t apply to people who already have reasonable glucose control, and/or doesn’t provide clear, actionable, conclusions.
So, I’ve decided to start experimenting on myself to try to better understand diabetes and how to manage it. In particular, I’d like to understand how different external stimuli (food, sleep, exercise, etc.) affect blood sugar levels. My goal is more than just optimization of my own diabetes management, I’d like to try to understand better how diabetes works and hopefully come up with better ways of managing it for everyone. Doing that will require getting others involved to pool data and brainpower.
That’s where this blog comes in. I’m going to post all my experiments here with detailed protocols, results, and analysis. The hope being that others will read it and be able to conduct their own experiments and analysis. If I’m really lucky, maybe we can create a community of diabetes self-trackers that can work together to better understand the disease.
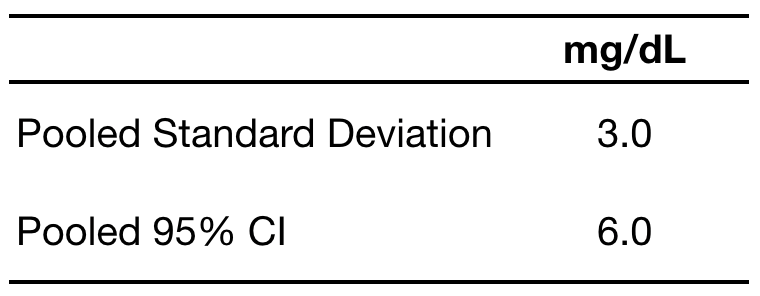
To start with, I’m going to post once each week. Next week, I’ll start with my first experiments to assess the precision and accuracy of my blood glucose measurements.
– QD